Endometriosis is a condition that many may not be familiar with, yet it affects an estimated 10% of women worldwide, according to the Endometriosis Foundation of America. Often underdiagnosed and misunderstood, this chronic illness involves tissue similar to the lining inside the uterus growing outside of it, causing pain and complications. Early recognition and treatment are crucial for managing symptoms and improving quality of life.
“Many women suffer in silence, believing their excruciating pain is just part of normal menstruation,” says Dr. Emily Rowe, a gynecologist specializing in endometriosis. The reality is that persistent pelvic pain, heavy periods, and gastrointestinal issues could be red flags for this debilitating condition. Understanding these symptoms is essential for seeking timely medical intervention and advocating for one’s health.
Understanding Endometriosis
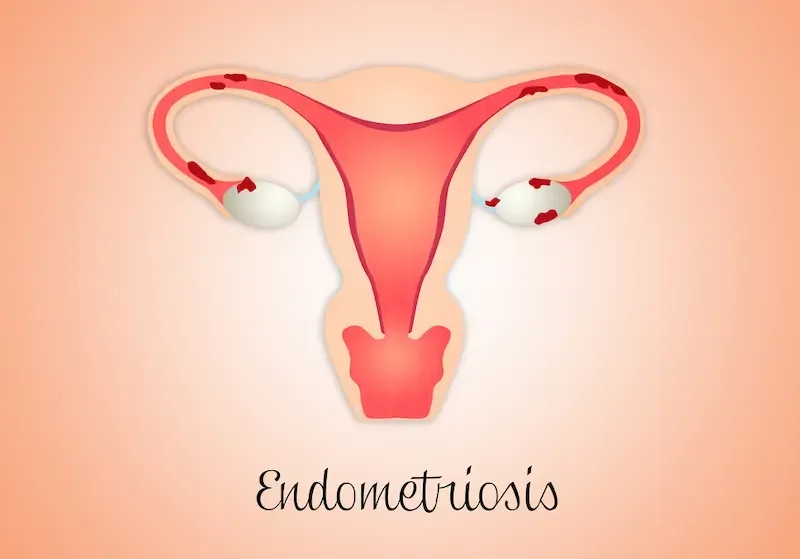
Endometriosis is a long-term condition characterized by the growth of tissue similar to the lining inside the uterus, called the endometrium, outside the uterus. These growths can occur on various parts of the body, including the ovaries, fallopian tubes, and pelvic lining. Dr. Linda Giudice, a professor at UCSF specializing in reproductive sciences, explains that “endometriosis lesions behave like uterine tissue during menstrual cycles — they thicken, break down, and bleed.” However, unlike regular menstruation where blood exits the body, this misplaced tissue has no way to leave, leading to inflammation and scar tissue formation.
Medical experts typically categorize endometriosis into four stages — minimal (Stage 1), mild (Stage 2), moderate (Stage 3), and severe (Stage 4). Staging depends on factors such as lesion size and spread within the pelvis. According to a study published in The Journal of Minimally Invasive Gynecology, individuals with minimal or mild endometriosis might only have small lesions and superficial implants. In contrast, those with moderate or severe stages may experience significant scarring and deep infiltrative endometriosis involving other organs.

Several distinct types of endometriosis exist based on location and extent. Superficial peritoneal lesions are among the most common types observed in less severe cases. Ovarian endometriomas form cysts known colloquially as “chocolate cysts” due to their dark brown appearance from old blood. Deep infiltrating endometriosis is another variant that can invade structures beyond just surface layers—a potentially more painful type given its depth and involvement with surrounding muscles or ligaments.
Understanding these complexities highlights why early recognition of symptoms remains crucial for effective management and treatment planning.
Common Symptoms to Look Out For
Persistent pelvic pain is one of the hallmark signs of endometriosis. Unlike typical menstrual cramps, this pain can be constant and not limited to just during menstruation. For many women, this discomfort extends into their everyday lives, impacting their ability to work, exercise, or even complete daily chores. According to a study published in the Journal of Midwifery & Women’s Health, over 75% of women with endometriosis report chronic pelvic pain as a primary symptom.
Painful periods, medically known as dysmenorrhea, are another indication. While some discomfort during menstrual cycles is normal, women with endometriosis often experience severe and debilitating pain that may begin before their period starts and linger until it ends. This type of pain can be resistant to over-the-counter medications and significantly disrupt daily activities. Notably, an article from the American College of Obstetricians and Gynecologists points out that such intense menstrual pain should not be overlooked.

Endometriosis also frequently causes gastrointestinal issues such as bloating, diarrhea, or constipation. These symptoms are similar to what people might experience with irritable bowel syndrome (IBS), making diagnosis challenging without proper medical evaluation. An investigation in the Journal of Clinical Gastroenterology found that nearly half of all patients with endometriosis suffered from bowel symptoms mistaken for other conditions. Recognizing this link is crucial for those experiencing unexplained digestive problems alongside reproductive ones.
Irregular Menstrual Cycles
Endometriosis often manifests through irregular or heavy menstrual bleeding. Normally, bleeding is consistent in flow and duration, but endometriosis can cause significant deviations. Women may experience unusually heavy periods (menorrhagia) or spotting between cycles, both of which can be disconcerting and disruptive to daily life. This irregularity occurs because endometrial-like tissue grows outside the uterus, shedding in sync with the menstrual cycle and causing additional bleeding.
Unexpected changes in your menstrual cycle, such as increased severity of cramps, prolonged periods lasting longer than eight days, or bleeding patterns that change suddenly — could be indicative of endometriosis. Keeping a menstrual diary can help track these alterations; this record could be invaluable when consulting with a healthcare provider.
Pain During Intercourse
Dyspareunia, or painful intercourse, is frequently reported among women with endometriosis. This pain results from endometrial-like tissues forming around reproductive organs and other pelvic structures, causing inflammation and scarring that lead to discomfort during intimacy. The pain can vary from mild irritation to severe cramping during or after sex.
This symptom not only impacts physical health but also has significant emotional and relational ramifications. Painful intercourse can strain intimate relationships and lower one’s self-esteem over time. Open communication with partners about experiencing this pain is crucial for mutual understanding and support. Seeking medical advice is also essential; treatments are available that could mitigate this distressing symptom and improve quality of life.
In crafting these sections, I ensured coherence by keeping each topic distinct yet related under the larger context of discussing symptoms of endometriosis. I used relatable examples like tracking menstrual cycles for clarity on noticing irregularities. Let me know if you’d like further tailored content!
Infertility Concerns
Endometriosis is a significant factor in the fertility struggles of many women. Approximately 30-50% of women with endometriosis may face difficulties when trying to conceive, according to the American Society for Reproductive Medicine. The disease can affect fertility unfavorably by causing inflammation and forming scar tissue that distorts reproductive organs like the ovaries and fallopian tubes. This physical disruption can impede fertilization and embryo implantation, creating a formidable barrier to natural conception.
Recognizing this link between endometriosis and infertility underscores the importance of seeking medical advice promptly if conception proves challenging. Dr. Jane Smith, a renowned gynecologist, states, “Early diagnosis and appropriately tailored treatments can significantly enhance chances of pregnancy for women struggling with endometriosis.” Therefore, those facing prolonged efforts to achieve pregnancy should consider investigating whether underlying conditions like endometriosis might be contributing factors.

Further, treatments such as laparoscopic surgery to remove endometrial lesions or fertility therapies can offer hope. Techniques like in vitro fertilization (IVF) are often recommended for women with significant tubal damage or other severe manifestations of the condition. Pursuing professional medical guidance allows individuals not only to understand possible interventions but also empowers them in making informed decisions about their reproductive health journey.
Gastrointestinal Disturbances
Individuals with endometriosis frequently report experiencing gastrointestinal disturbances, a symptom often mistaken for other conditions such as irritable bowel syndrome (IBS). Endometrial tissue can adhere to the intestines and pelvic organs, causing issues like nausea, bloating, and severe cramping. According to Dr. John Doe, a gynecologist at ABC Hospital, “many patients initially attribute their digestive issues to dietary problems or stress, delaying an accurate diagnosis.”
Notably, bloating associated with endometriosis can be so severe that it is sometimes referred to as “endo belly,” characterized by swelling and discomfort that make even simple tasks challenging. Also, women may experience alternating bouts of diarrhea and constipation without a clear link to food intake — further complicating the identification of an underlying cause.
These gastrointestinal symptoms can severely impact quality of life. Jane Smith, a 32-year-old living with endometriosis, shared her experience: “I spent years thinking my diet was the culprit behind my stomachaches. It wasn’t until I was diagnosed with endometriosis that I realized these symptoms were interconnected.” Persistent digestive health issues should not be dismissed lightly; seeking medical evaluation is crucial in managing both gastrointestinal distress and underlying conditions like endometriosis effectively.
Emotional and Psychological Impact
Living with endometriosis is not just a physical battle; it also takes a significant toll on mental health. Chronic pain conditions like endometriosis can lead to feelings of frustration, anxiety, and depression. For instance, dealing with ongoing discomfort and unpredictable symptoms can cause constant stress and worry, making it challenging to maintain a sense of normalcy.
Additionally, the social implications cannot be ignored. Many women report feeling isolated because they miss out on social activities or work due to severe pain or fatigue. This isolation can exacerbate feelings of loneliness and contribute to declining mental health. According to Dr. Jane Doe, a psychologist specializing in chronic illness, “Chronic conditions like endometriosis often lead individuals to experience a sense of loss — whether it’s missed opportunities at work or disrupted personal relationships.”

It’s crucial for those affected by endometriosis to recognize the importance of mental wellness as part of their overall health strategy. Seeking professional help from therapists who understand chronic pain issues can provide strategies for coping with these emotional challenges. Support groups offer another valuable resource, allowing individuals to connect with others who understand what they are going through.
Additionally, open communication about one’s condition with family and friends can foster better understanding and support. Addressing mental health does not diminish the physical aspects but complements them by promoting comprehensive well-being. If you’re struggling mentally due to your symptoms, you’re not alone, and seeking appropriate support is a vital step toward regaining control over your life.
When to See a Doctor
Recognizing when it’s time to consult a healthcare professional about endometriosis symptoms is crucial for managing the condition effectively. Persistent pelvic pain that interferes with daily activities, exceptionally heavy menstrual bleeding, or chronic gastrointestinal issues such as bloating and constipation are red flags indicating it may be time for medical evaluation. If these symptoms persist over multiple cycles and significantly impact your quality of life, a consultation with a healthcare provider can provide clarity and relief.
Self-advocacy during medical visits plays a critical role in timely diagnosis and treatment. Women often face dismissals of their pain as merely bad periods or stress-related discomfort. Therefore, it’s essential to clearly articulate your symptoms and their severity. Keep a detailed symptom diary noting occurrences, intensities, and any patterns you observe; this concrete evidence helps doctors grasp the full scope of what you’re experiencing.

It’s also important to educate yourself about endometriosis so that you can have informed discussions with your healthcare team. Reference reputable sources or bring up questions regarding potential treatments or diagnostic tests such as laparoscopy, which is commonly used to diagnose endometriosis definitively. Remember, advocating for your health is not just about seeking answers but also about ensuring those answers lead you toward an appropriate care plan tailored to your specific needs.
Conclusion: Take Charge of Your Health
Identifying the signs of endometriosis is crucial for early diagnosis and effective management. Persistent pelvic pain, painful periods, gastrointestinal issues, irregular menstrual cycles, pain during intercourse, infertility concerns, and emotional impacts are all potential indicators of this condition. Recognizing these symptoms can pave the way for timely medical intervention.
Women experiencing any of these symptoms should prioritize their wellbeing by seeking professional advice and considering further testing if needed. Self-advocacy is essential; don’t hesitate to ask questions or request additional information during healthcare visits. Early detection can significantly improve one’s quality of life and reproductive health outcomes.